PRI COVID-19 Update: Preparations for Opening Up Your Practice
PRI COVID-19 Update Preparations for Opening Up Your Practice
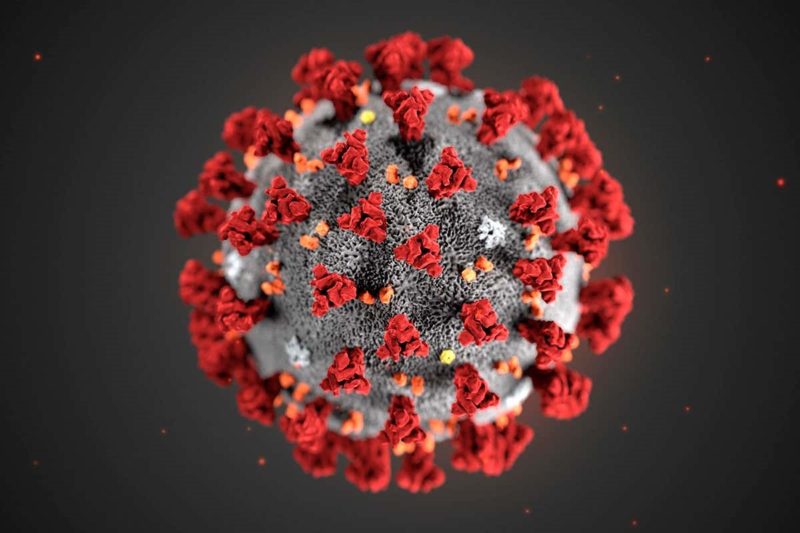 Physicians’ Reciprocal Insurers (PRI) would like to update our insured doctors and facility managers regarding evolving malpractice issues associated with COVID-19. As restrictions begin to lift and practices look to transition to a higher percentage of in-person care, providers should be aware of associated risks.
Physicians’ Reciprocal Insurers (PRI) would like to update our insured doctors and facility managers regarding evolving malpractice issues associated with COVID-19. As restrictions begin to lift and practices look to transition to a higher percentage of in-person care, providers should be aware of associated risks.
One area of confusion concerns the New York Governor’s Executive Orders and the Emergency or Disaster Treatment Protection Act which are intended to grant health care facilities and professionals immunity for care rendered during this public health emergency. Doctors and facility managers should be aware that neither the executive orders nor the legislation prevents patients from initiating lawsuits and that there are exceptions to the immunity, such as conduct constituting gross negligence or reckless misconduct.
10 Recommendations for Opening Up Your Practice
- Follow officially promulgated guidance for reopening practices such as the AMA’s COVID-19: A Physician Practice Guide to Reopening. For surgical and procedural practices, the American College of Surgeons has created helpful resources such as The American College of Surgeons Post-COVID-19 Readiness Checklist for Resuming Surgery. Dentists may refer to organizations such as the ADA as well as New York State’s Interim Guidance for Dentistry During the COVID-19 Public Health Emergency.
- If you have modified your malpractice coverage during quarantine, ensure that your coverage is appropriate in advance of gearing back up to full practice.
- Implement updated infection control policies such as the CDC’s Infection Control Guidance for Healthcare Professionals about Coronavirus (COVID-19) and OSHA’s Guidance on Preparing Workplaces for COVID-19 Situation
- If you have adopted telemedicine services during quarantine, ensure that those records are available to you when transitioning back to in-person patient care.
- It is natural for your staff to be worried and fearful and to look to you for leadership. Have frequent team meetings with your staff to reacquaint the team back to the office setting and review any changes and updates to workflows and policies. Elicit and address staff concerns. Consider use of simulation training with staff, particularly when new workflows are involved and to provide a refresher for existing office procedures.
- Know your supply chains to ensure that needed medical supplies are available. For personal protective equipment (PPE), refer to CDC recommendations – CDC Strategies to Optimize the Supply of PPE and Equipment
- Communicate with your network of specialty providers to whom you commonly refer patients to determine when and how you will be able to refer patients to needed services. Referring patients to services that are not available can lead to frustration and diagnostic/treatment delays.
- Be aware of cognitive biases during the COVID-19 pandemic. For example, doctors should continue to be on the alert for other potential problems that could be construed as COVID-19. Therefore, it is important to generate a broad differential diagnosis of COVID associated symptoms including atypical manifestations of common diseases as well as uncommon etiologies. It is important to document a differential diagnosis along with clinical reasoning associated with medical decision-making.
- Be aware of affective biases during the COVID-19 pandemic. Patients and providers alike have conditioned behaviors related to COVID-19 such as social distancing. When in-person elective care resumes to more normal levels, these conditioned behaviors may adversely affect in-person history gathering, physical examination, and patient compliance with follow-up and referrals. It is important to consider these issues, to document reasons for deferring in-person care, and to document any patient compliance issues. For example, if a patient refuses referral to the ED for a non-COVID related condition, it is important to document these refusals, as well as any informed consent conversation related to the refusal. Where appropriate, use telemedicine services for follow-up and to manage chronic conditions, particularly in vulnerable patients where sustained quarantine is necessary.
- Try to recognize the positives. While this pandemic has led to trauma, suffering, and loss, many doctors have missed interacting with their patients during quarantine and are looking forward to seeing their patients again. At the same time, the public has a heightened appreciation for the tremendous services our physicians provide. You may wish to embrace opportunities for professional renewal as you look to transition back to in-person patient care.
THIS MATERIAL IS PROVIDED FOR INFORMATIONAL PURPOSES AND IS NOT TO BE CONSTRUED AS DICTATING THE PRACTICE OF MEDICINE.

